Step-by-step of Ultrasound-guided Core-needle Biopsy of the Breast Review and Technique
Ultrasound-Guided Chest Biopsy
An ultrasound-guided chest biopsy uses audio waves to help locate a lump or abnormality and remove a tissue sample for test under a microscope. It is less invasive than surgical biopsy, leaves lilliputian to no scarring and does not involve exposure to ionizing radiation.
Tell your physician about whatever recent illnesses or medical conditions and whether y'all accept any allergies, especially to anesthesia. Discuss any medications you're taking, including herbal supplements and aspirin. You lot will be advised to stop taking aspirin or claret thinner three days earlier your procedure. Exit jewelry at domicile and wear loose, comfortable clothing. Y'all may be asked to wear a gown. If you are to be sedated, program to accept someone drive y'all home afterward.
- What is Ultrasound-Guided Breast Biopsy?
- What are some common uses of the procedure?
- How should I ready?
- What does the equipment look like?
- How does the procedure work?
- How is the procedure performed?
- What volition I feel during and afterwards the procedure?
- Who interprets the results and how do I get them?
- What are the benefits vs. risks?
- What are the limitations of Ultrasound-Guided Breast Biopsy?
What is Ultrasound-Guided Chest Biopsy?
Physical, mammography, and other exams frequently discover lumps or abnormalities in the breast. However, these tests cannot ever tell whether a growth is benign or cancerous.
Doctors use chest biopsy to remove a small corporeality of tissue from a suspicious area for lab analysis. The doctor may perform a biopsy surgically. More unremarkably, a radiologist volition use a less invasive procedure that involves a hollow needle and image-guidance. Image-guided needle biopsy does not remove the entire lesion. Instead, it obtains a pocket-sized sample of the abnormality for farther assay.
Image-guided biopsy uses ultrasound, MRI, or mammography imaging guidance to take samples of an abnormality.
In ultrasound-guided breast biopsy, ultrasound imaging is used to aid guide the radiologist'due south instruments to the site of the abnormal growth.
top of page
What are some common uses of the procedure?
An ultrasound-guided breast biopsy can exist performed when a breast ultrasound shows an abnormality such as:
- a suspicious solid mass
- a distortion in the structure of the breast tissue
- an area of abnormal tissue change
In that location are times when your doctor may decide that ultrasound guidance for biopsy is appropriate even for a mass that tin be felt.
Ultrasound guidance is used in four biopsy procedures:
- fine needle aspiration (FNA), which uses a very pocket-size needle to excerpt fluid or cells from the abnormal area.
- core needle (CN), which uses a large hollow needle to remove one sample of breast tissue per insertion.
- vacuum-assisted device (VAD), which uses a vacuum powered instrument to collect multiple tissue samples during one needle insertion.
- wire localization, in which a guide wire is placed into the suspicious area to aid the surgeon locate the lesion for surgical biopsy.
top of page
How should I prepare?
Wearable comfortable, loose-fitting clothing. You may need to remove all clothing and jewelry in the area to be examined.
You may need to change into a gown for the process.
Prior to a needle biopsy, tell your md about all the medications you have, including herbal supplements. List any allergies, especially to anesthesia. Your doctor may propose you to stop taking aspirin, blood thinners, or certain herbal supplements iii to 5 days before your procedure. This will aid decrease your risk of haemorrhage.
Too, inform your medico about recent illnesses or other medical weather condition.
You lot may want to have someone bulldoze you dwelling afterward, especially if you receive sedation.
tiptop of page
What does the equipment wait like?
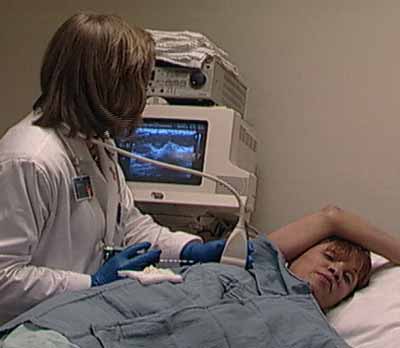
Ultrasound machines consist of a figurer panel, video monitor and an attached transducer. The transducer is a modest paw-held device that resembles a microphone. Some exams may use different transducers (with unlike capabilities) during a single examination. The transducer sends out inaudible, high-frequency sound waves into the trunk and listens for the returning echoes. The same principles apply to sonar used by boats and submarines.
The technologist applies a modest amount of gel to the area under exam and places the transducer there. The gel allows sound waves to travel dorsum and forth between the transducer and the surface area under test. The ultrasound image is immediately visible on a video monitor. The reckoner creates the image based on the loudness (amplitude), pitch (frequency), and fourth dimension it takes for the ultrasound signal to return to the transducer. It also considers what type of torso construction and/or tissue the sound is traveling through.
The dr. will use ane of four instruments:
- A fine needle fastened to a syringe, smaller than needles typically used to describe claret.
- A core needle, also called an automatic, spring-loaded needle, which consists of an inner needle connected to a trough, or shallow receptacle, covered past a sheath and attached to a jump-loaded mechanism.
- A vacuum-assisted device (VAD), a vacuum-powered instrument that uses pressure to pull tissue into the needle.
- A thin guide wire, which is used for a surgical biopsy.
This procedure may use other sterile equipment, including syringes, sponges, forceps, scalpels, and a specimen cup or microscope slide.
summit of page
How does the procedure work?
Ultrasound imaging uses the aforementioned principles as the sonar that bats, ships, and fishermen use. When a sound wave strikes an object, it bounces back or echoes. By measuring these echo waves, information technology is possible to determine how far away the object is as well as its size, shape, and consistency. This includes whether the object is solid or filled with fluid.
Doctors use ultrasound to detect changes in the appearance of organs, tissues, and vessels and to detect abnormal masses, such as tumors.
In an ultrasound examination, a transducer both sends the sound waves and records the echoing (returning) waves. When the transducer is pressed against the skin, it sends small pulses of inaudible, high-frequency sound waves into the body. Every bit the sound waves bounce off internal organs, fluids and tissues, the sensitive receiver in the transducer records tiny changes in the sound's pitch and direction. A computer instantly measures these signature waves and displays them as real-time pictures on a monitor. The technologist typically captures one or more frames of the moving pictures as nevertheless images. They may likewise save short video loops of the images.
Using an ultrasound probe to visualize the location of the chest mass, distortion or aberrant tissue alter, the radiologist inserts a biopsy needle through the skin, advances it into the targeted finding and removes tissue samples. If a surgical biopsy is existence performed, ultrasound may exist used to guide a wire directly into the targeted finding to help the surgeon locate the area for excision. With continuous ultrasound imaging, the doctor is able to view the biopsy needle or wire as it advances to the location of the lesion in real-fourth dimension.
summit of page
How is the procedure performed?
Image-guided, minimally invasive procedures such every bit ultrasound-guided chest biopsy are virtually often performed by a peculiarly trained radiologist.
Breast biopsies are usually done on an outpatient basis.
You will be positioned lying face upwards on the examination table or turned slightly to the side.
The doctor will inject a local anesthetic into the skin and more securely into the breast to numb it.
Pressing the transducer to the breast, the sonographer or radiologist will locate the lesion.
The doctor will make a very small-scale nick in the skin at the site where they will insert the biopsy needle.
The radiologist, monitoring the lesion site with the ultrasound probe, volition insert the needle and advance information technology directly into the mass.
The physician removes tissue samples using 1 of three methods:
- In a fine needle aspiration, a fine estimate needle and a syringe withdraw fluid or clusters of cells.
- In a cadre needle biopsy, the automated mechanism is activated, moving the needle forrad and filling the needle trough, or shallow receptacle, with "cores" of breast tissue. The outer sheath instantly moves forward to cut the tissue and go on it in the trough. The doctor repeats this process 3 to six times.
- With a vacuum-assisted device (VAD), vacuum pressure pulls tissue from the breast through the needle into the sampling sleeping accommodation. Without withdrawing and reinserting the needle, it rotates positions and collects boosted samples. Typically, the doctor volition collect 8 to 10 samples of tissue from around the lesion.
After this sampling, the doctor will remove the needle.
If a surgical biopsy is to exist performed, the dr. will insert a wire into the suspicious area as a guide for the surgeon.
The doctor may place a small marker at the biopsy site so they can locate information technology in the futurity if necessary.
One time the biopsy is consummate, the physician or nurse will apply pressure to stop whatever bleeding. They will encompass the opening in the skin with a dressing. No sutures are needed.
The doctor may utilise mammography to confirm that the marker is in the proper position.
This procedure is usually completed within an hour.
top of folio
What will I feel during and later on the procedure?
You volition exist awake during your biopsy and should have little discomfort. Many women report niggling pain and no scarring on the breast. Withal, certain patients, including those with dumbo breast tissue or abnormalities near the chest wall or behind the nipple, may be more sensitive during the procedure.
When y'all receive the local anesthetic to numb the peel, you will feel a pivot prick from the needle followed past a balmy stinging sensation from the local coldhearted. You will likely feel some pressure when the doc inserts the biopsy needle and during tissue sampling. This is normal.
The area will go numb inside a few seconds.
You must remain very still while the dr. performs the imaging and the biopsy.
As tissue samples are taken, you may hear clicks or buzzing sounds from the sampling instrument. These are normal.
If you experience swelling and bruising following your biopsy, your md may tell yous to take an over-the-counter pain reliever and to apply a cold pack. Temporary bruising is normal.
Telephone call your doc if you feel excessive swelling, haemorrhage, drainage, redness, or heat in the breast.
If a marking is left inside the breast to marking the location of the biopsied lesion, it will cause no pain, disfigurement, or impairment. Biopsy markers are MRI uniform and will not cause metallic detectors to alarm.
Avoid strenuous activity for at to the lowest degree 24 hours after the biopsy. Your doc volition outline more detailed post-procedure care instructions for yous.
top of page
Who interprets the results and how practice I get them?
A pathologist examines the removed specimen and makes a final diagnosis. Depending on the facility, the radiologist or your referring dr. volition share the results with you lot. The radiologist will also evaluate the results of the biopsy to brand sure that the pathology and image findings explicate ane some other. In some instances, even if cancer is non diagnosed, surgical removal of the entire biopsy site and imaging aberration may be recommended if the pathology does non match the imaging findings.
Yous may demand a follow-up exam. If and so, your doctor will explain why. Sometimes a follow-up examination farther evaluates a potential issue with more views or a special imaging technique. It may too see if there has been whatever change in an issue over time. Follow-up exams are oft the best style to see if treatment is working or if a problem needs attention.
top of page
What are the benefits vs. risks?
Benefits
- The process is less invasive than surgical biopsy, leaves fiddling or no scarring, and can be performed in less than an hour.
- Ultrasound imaging uses no ionizing radiation.
- Ultrasound-guided breast biopsy reliably provides tissue samples that tin prove whether a breast lump is beneficial or malignant.
- Compared with stereotactic breast biopsy, the ultrasound method is faster and avoids the need for ionizing radiation exposure.
- With ultrasound information technology is possible to follow the motility of the biopsy needle as it moves through the breast tissue.
- Ultrasound-guided breast biopsy is able to evaluate lumps under the arm or near the chest wall, which are hard to reach with stereotactic biopsy.
- Ultrasound-guided biopsy is less expensive than other biopsy methods, such as open surgical biopsy or stereotactic biopsy. CMID6019
Risks
- There is a risk of haemorrhage and forming a hematoma, or a drove of blood at the biopsy site. The run a risk, however, appears to be less than 1 percent of patients.
- An occasional patient has meaning discomfort, which tin be readily controlled by non-prescription hurting medication.
- Any procedure where the peel is penetrated carries a risk of infection. The chance of infection requiring antibody handling appears to be less than one in 1,000.
- Depending on the type of biopsy or the design of the biopsy machine, a biopsy of tissue located deep within the breast carries a slight risk that the needle will pass through the breast wall. This could permit air around the lung and cause the lung to collapse. This is extremely rare.
- In that location is a small chance that this procedure will not provide the final reply to explicate the imaging abnormality.
top of page
What are the limitations of Ultrasound-Guided Breast Biopsy?
Chest biopsy procedures will occasionally miss a lesion or underestimate the extent of affliction nowadays. If the diagnosis remains uncertain after a technically successful procedure, surgical biopsy will usually be necessary.
The ultrasound-guided biopsy method cannot exist used unless the lesion can exist seen on an ultrasound test. Clustered calcifications are not shown equally clearly with ultrasound equally with x-rays.
Very minor lesions may be hard to target accurately by ultrasound-guided core biopsy.
top of page
This page was reviewed on July, 20, 2021
Images
Sponsored Past


Please note
RadiologyInfo.org is not a medical facility. Please contact your physician with specific medical questions or for a referral to a radiologist or other doc. To locate a medical imaging or radiation oncology provider in your community, you can search the ACR-accredited facilities database.
This website does not provide cost information. The costs for specific medical imaging tests, treatments and procedures may vary by geographic region. Hash out the fees associated with your prescribed procedure with your doctor, the medical facility staff and/or your insurance provider to go a better agreement of the possible charges you will incur.
Web page review process: This Web page is reviewed regularly by a physician with expertise in the medical surface area presented and is further reviewed by committees from the Radiological Gild of North America (RSNA) and the American College of Radiology (ACR), comprising physicians with expertise in several radiologic areas.
Outside links: For the convenience of our users, RadiologyInfo.org provides links to relevant websites. RadiologyInfo.org, RSNA and ACR are not responsible for the content contained on the spider web pages institute at these links.
Source: https://www.radiologyinfo.org/en/info/breastbius
0 Response to "Step-by-step of Ultrasound-guided Core-needle Biopsy of the Breast Review and Technique"
Post a Comment